
These practical tips can help you make healthier choices. The two
keys to a healthy
diet are eating the right amount of food for how
active you are and eating a range of foods to make sure you're getting a
balanced diet.
A healthy balanced diet contains a variety of
types of food, including lots of fruit, vegetables and starchy foods
such as wholemeal bread and wholegrain cereals; some protein-rich foods
such as meat, fish, eggs and lentils; and some milk and dairy foods.
On this page
1. Base your meals on starchy foods
2. Eat lots of fruit and veg
3. Eat more fish
4. Cut down on saturated fat and sugar
5. Try to eat less salt - no more than 6g a day
6. Get active and try to be a healthy weight
7. Drink plenty of water
8. Don't skip breakfast
1. Base your meals on starchy foods

Starchy foods such as bread, cereals, rice, pasta and
potatoes are a really important part of a healthy diet. Try to choose
wholegrain varieties of starchy foods whenever you can.
Starchy
foods should make up about a third of the food we eat. They are a good
source of energy and the main source of a range of
nutrients in our
diet. As well as starch, these foods contain fibre, calcium, iron and B
vitamins.
Most of us should eat more starchy foods - try to include
at least one starchy food with each of your main meals. So you could
start the day with a wholegrain breakfast cereal, have a sandwich for
lunch, and potatoes, pasta or rice with your evening meal.
Some
people think starchy foods are fattening, but gram for gram they contain
less than half the calories of fat. You just need to watch the fats you
add when cooking and serving these foods, because this is what
increases the calorie content.
Why choose wholegrain foods?

Wholegrain foods contain more fibre and other nutrients than white or refined starchy foods.
We also digest wholegrain foods more slowly so they can help make us feel full for longer.
Wholegrain foods include:
- Wholemeal and wholegrain bread, pitta and chapatti
- Wholewheat pasta and brown rice
- Wholegrain breakfast cereals
2. Eat lots of fruit and veg

Most people know we should be eating more fruit and veg. But most of us still aren't eating enough.
Try to eat at least 5 portions of a variety of fruit and veg every day. It might be easier than you think.
You could try adding up your portions during the day.
For example, you could have:
- a glass of juice and a sliced banana with your cereal at breakfast
- a side salad at lunch
- a pear as an afternoon snack
- a portion of peas or other vegetables with your evening meal
You
can choose from fresh, frozen, tinned, dried or juiced, but remember
potatoes count as a starchy food, not as portions of fruit and veg.
3. Eat more fish

Most of us should be eating more fish - including a
portion of oily fish each week. It's an excellent source of protein and
contains many vitamins and minerals.
Aim for at least two
portions of fish a week, including a portion of oily fish. You can
choose from fresh, frozen or canned - but remember that canned and
smoked fish can be high in salt.
What are oily fish?
Some fish are called oily fish because they are rich in
certain types of fats, called omega 3 fatty acids, which can help keep
our hearts healthy.
How much oily fish?
Although most of us should be eating more oily fish, women
who might have a baby one day should have a maximum of 2 portions of
oily fish a week (a portion is about 140g). And 4 is the recommended
maximum number of portions for other adults.
Examples of oily fish
Salmon, mackerel, trout, herring, fresh tuna, sardines, pilchards, eel
Examples of white or non-oily fish
Haddock, plaice, coley, cod, tinned tuna, skate, hake
Shark, swordfish and marlin
Don't have more than one portion a week of these types of fish. This is because of the high levels of mercury in these fish.
Anyone
who regularly eats a lot of fish should try to choose as wide a variety
as possible. Eating a wider variety of fish and shellfish will also
help reduce the environmental impact.
For more information on
fish and for advice - including recommended limits - for children, women
who are pregnant, breastfeeding or trying for a baby, see the link
below.
4. Cut down on saturated fat and sugar
Fats

To stay healthy we need some fat in our diets. What is
important is the kind of fat we are eating. There are two main types of
fat:
- saturated fat - having too much can increase the
amount of cholesterol in the blood, which increases the chance of
developing heart disease
- unsaturated fat - having unsaturated fat instead of saturated fat lowers blood cholesterol
Try
to cut down on food that is high in saturated fat and
have foods that
are rich in
unsaturated fat instead, such as vegetable
oils (including
sunflower, rapeseed and
olive oil), oily fish, avocados, nuts and seeds.
Foods high in saturated fat
Try to eat these sorts of foods less often or in small amounts:
- meat pies, sausages, meat with visible white fat
- hard cheese
- butter and lard
- pastry
- cakes and biscuits
- cream, soured cream and crème fraîche
- coconut oil, coconut cream or palm oil
For
a healthy choice, use just a small amount of vegetable oil or a
reduced-fat spread instead of butter, lard or ghee. And when you are
having meat, try to choose lean cuts and cut off any visible fat.
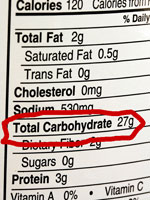
How do I know if a food is high in fat?
Look at the label to see how much fat a food contains.
Generally the label will say how many grams (g) of fat there are in 100g
of the food.
Some foods also give a figure for saturated fat, or 'saturates'.
Use the following as a guide to work out if a food is high or low in fat.
Total fat - what's high and what's low?
High is more than 20g fat per 100g
Low is 3g fat or less per 100g
If the amount of fat per 100g is in between these figures, then that is a
medium level of fat.
Saturated fat - what's high and what's low?
High is more than 5g saturates per 100g
Low is 1.5g saturates or less per 100g
If the amount of saturates per 100g is in between these figures, then that is a medium level of saturated fat.
Remember that the amount you eat of a particular food affects how much fat you will get from it.
Try to choose more
foods that are low in fat and cut down on foods that are high in fat.
Sugar

Most people in the UK are eating too much sugar. We should
all be trying to eat fewer foods containing added sugar, such as
sweets, cakes and biscuits, and drinking fewer sugary soft and fizzy
drinks.
Having sugary foods and drinks too often can cause
tooth
decay, especially if you have them between meals. Many foods that
contain added sugar can also be high in calories so cutting down could
help you control your weight.
How do I know if a food is high in added sugar?
Take a look at the label. The ingredients list always starts with the biggest ingredient first.
But
watch out for other words used to describe added sugars, such as
sucrose, glucose, fructose, maltose, hydrolysed starch and invert sugar,
corn syrup and honey. If you see one of these near the top of the list,
you know the food is likely to be high in added sugars.
Another
way to get an idea of how much sugar is in a food is to have a look for
the 'Carbohydrates (of which sugars)' figure on the label. But this
figure can't tell you how much is from added sugars, which is the type
we should try to cut down on.
High is more than 15g sugars per 100g
Low is 5g sugars or less per 100g
If the amount of sugars per 100g is in between these figures, then that is a medium level of sugars.
Remember that the amount you eat of a particular food affects how much sugars you will get from it.
Sometimes
you will only see a figure for total 'Carbohydrates', not for
'Carbohydrates (of which sugars)', which means the figure also includes
the carbohydrate from starchy foods.
5. Try to eat less salt - no more than 6g a day

Lots of people think they don't eat much salt, especially
if they don't add it to their food. But don't be so sure!
Every
day in the UK, 85% men and 69% women eat too much salt. Adults - and
children over 11 - should have no more than 6g salt a day. Younger
children should have even less.
Three-quarters (75%) of the salt
we eat is already in the food we buy, such as breakfast cereals, soups,
sauces and ready meals. So you could easily be eating too much salt
without realising it.
Eating too much salt can raise your blood
pressure. And people with high blood pressure are three times more
likely to develop heart disease or have a stroke than people with normal
blood pressure.
How do I know if a food is high in salt?
Check the label to find out the figure for salt per 100g.
High is more than 1.5g salt per 100g (or 0.6g sodium)
Low is 0.3g salt or less per 100g (or 0.1g sodium)
If the amount of salt per 100g is in between these figures, then that is a medium level of salt.
Remember that the amount you eat of a particular food affects how much salt you will get from it.
6. Get active and try to be a healthy weight

It's not a good idea to be either underweight or
overweight. Being overweight can lead to health conditions such as heart
disease, high blood pressure or diabetes. Being underweight could also
affect your health.
Check if you are the right weight for your height using the link below.
If
you're worried about your weight, ask your GP or a dietitian for
advice. But if you think you just need to lose a little weight, the main
things to remember are:
- only eat as much food as you need
- make healthy choices - it's a good idea to choose low-fat and low-sugar varieties, eat plenty of fruit and veg and wholegrains
- get more active
It's also important to eat a variety of types of food so you get all the nutrients your body needs.
Physical
activity is a good way of using up extra calories, and helps control
our weight. But this doesn't mean you need to join a gym.
Just
try to get active every day and build up the amount you do. For example,
you could try to fit in as much walking as you can into your daily
routine. Try to walk at a good pace.
Whenever we eat more than
our body needs, we put on weight. This is because we store any energy we
don't use up - usually as fat. Even small amounts of extra energy each
day can lead to weight gain.
But crash diets aren't good for your
health and they don't work in the longer term. The way to reach a
healthy weight - and stay there - is to change your lifestyle gradually.
Aim to lose about 0.5 to 1kg (about 1 to 2lbs) a week, until you reach a
healthy weight for your height.
7. Drink plenty of water

We should be drinking about 6 to 8 glasses (1.2 litres) of
water, or other fluids, every day to stop us getting dehydrated.
When
the weather is warm or when we get active, our bodies need more than
this. But avoid drinking soft and fizzy drinks that are high in added
sugar.
Alcohol
There is nothing wrong with the occasional drink. But
drinking too much can cause problems. Alcohol is also high in calories,
so cutting down could help you control your weight.
Women can drink up to 2 to 3 units of alcohol a day and men up to 3 to 4 units a day, without significant risk to their health.
A
unit is half a pint of standard strength (3 to 5% ABV) beer, lager or
cider, or a pub measure of spirit. A glass of wine is about 2 units and
alcopops are about 1.5 units.
For good health, it's a good idea
to spread your drinking throughout the week and avoid binge drinking.
Drinking heavily over a long period of time can damage the liver.
8. Don't skip breakfast

Breakfast can help give us the energy we need to face the
day, as well as some of the vitamins and minerals we need for good
health.
Some people skip breakfast because they think it will
help them lose weight. But missing meals doesn't help us lose weight and
it isn't good for us, because we can miss out on essential nutrients.
There is some evidence to suggest that eating breakfast can actually help people control their weight.
So
why not go for a bowl of wholegrain cereal with some low-fat milk and
sliced banana and a glass of fruit juice for a healthy start to the day?










 These practical tips can help you make healthier choices. The two
keys to a healthy
These practical tips can help you make healthier choices. The two
keys to a healthy 

 Starchy foods such as bread, cereals, rice, pasta and
potatoes are a really important part of a healthy diet. Try to choose
wholegrain varieties of starchy foods whenever you can.
Starchy foods such as bread, cereals, rice, pasta and
potatoes are a really important part of a healthy diet. Try to choose
wholegrain varieties of starchy foods whenever you can.  Wholegrain foods contain more fibre and other nutrients than white or refined starchy foods.
Wholegrain foods contain more fibre and other nutrients than white or refined starchy foods. Most people know we should be eating more fruit and veg. But most of us still aren't eating enough.
Most people know we should be eating more fruit and veg. But most of us still aren't eating enough.  Most of us should be eating more fish - including a
portion of oily fish each week. It's an excellent source of protein and
contains many vitamins and minerals.
Most of us should be eating more fish - including a
portion of oily fish each week. It's an excellent source of protein and
contains many vitamins and minerals. To stay healthy we need some fat in our diets. What is
important is the kind of fat we are eating. There are two main types of
fat:
To stay healthy we need some fat in our diets. What is
important is the kind of fat we are eating. There are two main types of
fat: Most people in the UK are eating too much sugar. We should
all be trying to eat fewer foods containing added sugar, such as
sweets, cakes and biscuits, and drinking fewer sugary soft and fizzy
drinks.
Most people in the UK are eating too much sugar. We should
all be trying to eat fewer foods containing added sugar, such as
sweets, cakes and biscuits, and drinking fewer sugary soft and fizzy
drinks. Lots of people think they don't eat much salt, especially
if they don't add it to their food. But don't be so sure!
Lots of people think they don't eat much salt, especially
if they don't add it to their food. But don't be so sure!  It's not a good idea to be either underweight or
overweight. Being overweight can lead to health conditions such as heart
disease, high blood pressure or diabetes. Being underweight could also
affect your health.
It's not a good idea to be either underweight or
overweight. Being overweight can lead to health conditions such as heart
disease, high blood pressure or diabetes. Being underweight could also
affect your health.  We should be drinking about 6 to 8 glasses (1.2 litres) of
water, or other fluids, every day to stop us getting dehydrated.
We should be drinking about 6 to 8 glasses (1.2 litres) of
water, or other fluids, every day to stop us getting dehydrated.  Breakfast can help give us the energy we need to face the
day, as well as some of the vitamins and minerals we need for good
health.
Breakfast can help give us the energy we need to face the
day, as well as some of the vitamins and minerals we need for good
health.